
Applications for the LAMP Fellowship 2025-26 will open soon. Sign up here to be notified when the dates are announced.
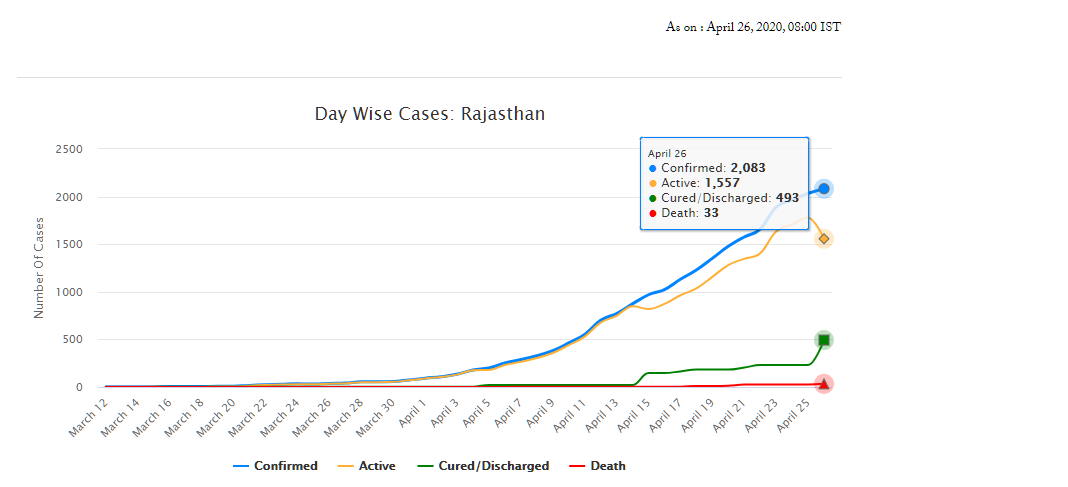
As of April 26, Rajasthan has 2,083 confirmed cases of COVID-19 (fifth highest in the country), of which 493 have recovered and 33 have died. On March 18, the Rajasthan government had declared a state-wide curfew till March 31, to check the spread of the disease. A nation-wide lockdown has also been in place since March 25 and is currently, extended up to May 3. The state has announced several policy decisions to prevent the spread of the virus and provide relief for those affected by it. This blog summarises the key policy measures taken by the Government of Rajasthan in response to the COVID-19 pandemic.
Early measures for containment
Between late January and early February, Rajasthan Government’s measures were aimed towards identification, screening and testing, and constant monitoring of passenger arrivals from China. Instructions were also issued to district health officials for various prevention, treatment, & control related activities, such as (i) mandatory 28-day home isolation for all travellers from China, (ii) running awareness campaigns, and (iii) ensuring adequate supplies of Personal Protection Equipments (PPEs). Some of the other measures, taken prior to the state-wide lockdown, are summarised below:
Administrative measures
The government announced the formation of Rapid Response Teams (RRTs), at the medical college-level and at district-level on March 3 and 5, respectively.
The District Collector was appointed as the Nodal Officer for all COVID-19 containment activities. Control Rooms were to be opened at all Sub-divisional offices. The concerned officers were also directed to strengthen information dissemination mechanisms and tackle the menace of fake news.
Directives were issued on March 11 to rural health workers/officials to report for duty on Gazetted holidays. Further, government departments were shut down between March 22 and March 31. Only essential departments such as Health Services were allowed to function on a rotation basis at 50% capacity and special / emergency leaves were permitted.
Travel and Movement
Air travellers were to undergo 14-day home isolation and were also required to provide an undertaking for the same. Besides, those violating the mandated isolation/quarantine were liable to be punished under Section. 188 of the Indian Penal Code. Penalties are imposed under this section on persons for the willful violation of orders that have been duly passed by a public servant.
All institutions and establishments, such as (i) educational institutions, theatres, and gyms, (ii) anganwadis, (iii) bars, discos, libraries, restaurants etc, (iv) museums and tourist places, were directed to be shut down till March 31.
The daily Jan Sunwai at the Chief Minister’s residence was cancelled until further notice. Various government offices were directed to shut down and exams of schools and colleges were postponed.
On March 24, the government issued a state-wide ban on the movement of private vehicles till March 31.
Health Measures
Advisories regarding prevention and control measures were issued to: (i) District Collectors, regarding sample collection and transportation, hotels, and preparedness of hospitals, (ii) Police department, to stop using breath analysers, (iii) Private hospitals, regarding preparedness and monitoring activities, and (iv) Temple trusts, to disinfect their premises with chemicals.
The government issued Standard Operating Procedures for conducting mock drills in emergency response handling of COVID-19 cases. Training and capacity building measures were also initiated for (i) Railways, Army personnel etc and (ii) ASHA workers, through video conferencing.
A model micro-plan for containing local transmission of COVID was released. Key features of the plan include: (i) identification and mapping of affected areas, (ii) activities for prevention control, surveillance, and contact tracing, (iii) human resource management, including roles and responsibilities, (iv) various infrastructural and logistical support, such as hospitals, labs etc, and (v) communication and data management.
Resource Management: Private hospitals and medical colleges were instructed to reserve 25 % of beds for COVID-19 patients. They were also instructed to utilise faculty from the departments of Preventive and Social Medicine to conduct health education and awareness activities.
Over 6000 Students of nursing schools were employed in assisting the health department to conduct screening activities being conducted at public places, railways stations, bus stands etc.
Further, the government issued guidelines to ensure the rational use of PPEs.
Welfare Measures
The government announced financial assistance, in the form of encouragement grants, to health professionals engaged in treating COVID-19 patients.
Steps were also taken by the government to ensure speedy disbursal of pensions for February and March.
The government also initiated the replacement of the biometric authentication with an OTP process for distribution of ration via the Public Distribution System (PDS).
During the lockdown
State-wide curfew announced on March 18 has been followed by a nation-wide lockdown between March 25 and May 3. However, certain relaxations have been recommended by the state government from April 21 onwards. Some of the key measures undertaken during the lockdown period are:
Administrative Measures
Advisory groups and task forces were set up on – (i) COVID-19 prevention, (ii) Health and Economy, and (iii) Higher education. These groups will provide advice on the way forward for (i) prevention and containment activities, (ii) post-lockdown strategies and strategies to revive the economy, and (iii) to address the challenges facing the higher education sector respectively.
Services of retiring medical and paramedical professionals retiring between March and August have been extended till September 2020.
Essential Goods and Services
A Drug Supply Control Room was set up at the Rajasthan Pharmacy Council. This is to ensure uninterrupted supply of medicines during the lockdown and will also assist in facilitating home delivery of medicines.
The government permitted Fair Price Shops to sell products such as masalas, sanitisers, and hygiene products, in addition to food grains.
Village service cooperatives were declared as secondary markets to facilitate farmers to sell their produce near their own fields/villages during the lockdown.
A Whatsapp helpline was also set up for complaints regarding hoarding, black marketing, and overpricing.
Travel and Movement
Once lockdown was in place, the government issued instructions to identify, screen, and categorise people from other states who have travelled to Rajasthan. They were to be categorised into: (i) people displaying symptoms to be put in isolation wards, (ii) people over 60 years of age with symptoms and co-morbidities to be put in quarantine centres, and (iii) asymptomatic people to be home quarantined.
On March 28, the government announced the availability of buses to transport people during the lockdown. Further, stranded students in Kota were allowed to return to their respective states.
On April 2, a portal and a helpline were launched to help stranded foreign tourists and NRIs.
On April 11, an e-pass facility was launched for movement of people and vehicles.
Health Measures
To identify COVID-19 patients, district officials were instructed to monitor people with ARI/URI/Pneumonia or other breathing difficulties coming into hospital OPDs. Pharmacists were also instructed to not issue medicines for cold/cough without prescriptions.
A mobile app – Raj COVID Info – was developed by the government for tracking of quarantined people. Quarantined persons are required to send their selfie clicks at regular intervals, failing which a notification would be sent by the app. The app also provides a lot of information on COVID-19, such as the number of cases, and press releases by the government.
Due to the lockdown, people had restricted access to hospitals and treatment. Thus, instructions were issued to utilise Mobile Medical Vans for treatment/screening and also as mobile OPDs.
On April 20, a detailed action plan for prevention and control of COVID-19 was released. The report recommended: (i) preparation of a containment plan, (ii) formation of RRTs, (iii) testing protocols, (iv) setting up of control room and helpline, (v) designated quarantine centres and COVID-19 hospitals, (vi) roles and responsibilities, and (vii) other logistics.
Welfare Measures
The government issued instructions to make medicines available free of cost to senior citizens and other patients with chronic illnesses through the Chief Minister’s Free Medicine Scheme.
Rs 60 crore was allotted to Panchayati Raj Institutions to purchase PPEs and for other prevention activities.
A one-time cash transfer of Rs 1000 to over 15 lakh construction workers was announced. Similar cash transfer of Rs 1000 was announced for poor people who were deprived of livelihood during the lockdown, particularly those people with no social security benefits. Eligible families would be selected through the Aadhaar database. Further, an additional cash transfer of Rs 1500 to needy eligible families from different categories was announced.
The state also announced an aid of Rs 50 lakh to the families of frontline workers who lose their lives due to COVID-19.
To maintain social distancing, the government will conduct a door-to-door distribution of ration to select beneficiaries in rural areas of the state. The government also announced the distribution of free wheat for April, May, and June, under the National Food Security Act, 2013. Ration will also be distributed to stranded migrant families from Pakistan, living in the state.
The government announced free tractor & farming equipment on rent in tie-up with farming equipment manufacturers to assist economically weak small & marginal farmers.
Other Measures
Education: Project SMILE was launched to connect students and teachers online during the lockdown. Study material would be sent through specially formed Whatsapp groups. For each subject, 30-40 minute content videos have been prepared by the Education Department.
Industry: On April 18, new guidelines were issued for industries and enterprises to resume operations from April 20 onwards. Industries located in rural areas or export units / SEZs in municipal areas where accommodation facilities for workers are present, are allowed to function. Factories have been permitted to increase the working hours from 8 hours to 12 hours per day, to reduce the requirement of workers in factories. This exemption has been allowed for the next three months for factories operating at 60% to 65% of manpower capacity.
For more information on the spread of COVID-19 and the central and state government response to the pandemic, please see here.
The Union Cabinet recently approved the launch of the National Health Protection Mission which was announced during Budget 2018-19. The Mission aims to provide a cover of five lakh rupees per family per year to about 10.7 crore families belonging to poor and vulnerable population. The insurance coverage is targeted for hospitalisation at the secondary and tertiary health care levels. This post explains the healthcare financing scenario in India, which is distributed across the centre, states, and individuals.
How much does India spend on health care financing vis-à-vis other countries?
The public health expenditure in India (total of centre and state governments) has remained constant at approximately 1.3% of the GDP between 2008 and 2015, and increased marginally to 1.4% in 2016-17. This is less than the world average of 6%. Note that the National Health Policy, 2017 proposes to increase this to 2.5% of GDP by 2025.
Including the private sector, the total health expenditure as a percentage of GDP is estimated at 3.9%. Out of the total expenditure, effectively about one-third (30%) is contributed by the public sector. This contribution is low as compared to other developing and developed countries. Examples include Brazil (46%), China (56%), Indonesia (39%), USA (48%), and UK (83%) (see Figure 1).

Who pays for healthcare in India? Mostly, it is the consumer out of his own pocket.
Given the public-private split of health care expenditure, it is quite clear that it is the private expenditure which dominates i.e. the individual consumer who bears the cost of her own healthcare. Let’s look at a further disaggregation of public spending and private spending to understand this.
In 2018-19, the Ministry of Health and Family Welfare received an allocation of Rs 54,600 crore(an increase of 2% over 2017-18). The National Health Mission (NHM) received the highest allocation at Rs 30,130 crore and constitutes 55% of the total Ministry allocation (see Table 1). Despite a higher allocation, NHM has seen a decline in the allocation vis-à-vis 2017-18.
Interestingly, in 2017-18, expenditure on NHM is expected to be Rs 4,000 crore more than what had been estimated earlier. This may indicate a greater capacity to spend than what was earlier allocated. A similar trend is exhibited at the overall Ministry level where the utilisation of the allocated funds has been over 100% in the last three years.
 State level spending
State level spending
A NITI Aayog report (2017) noted that low income states with low revenue capacity spend significant lower on social services like health. Further, differences in the cost of delivering health services have contributed to health disparities among and within states.
Following the 14th Finance Commission recommendations, there has been an increase in the states’ share in central pool of taxes and they were given greater autonomy and flexibility to spend according to their priorities. Despite the enhanced share of states in central taxes, the increase in health budgets by some states has been marginal (see Figure 2).
 Consumer level spending
Consumer level spending
If cumulatively 30% of the total health expenditure is incurred by the public sector, the rest of the health expenditure, i.e. approximately 70% is borne by consumers. Household health expenditures include out of pocket expenditures (95%) and insurance (5%). Out of pocket expenditure dominate and these are the payments made directly by individuals at the point of services which are not covered under any financial protection scheme. The highest percentage of out of pocket health expenditure (52%) is made towards medicines (see Figure 3).

This is followed by private hospitals (22%), medical and diagnostic labs (10%), and patient transportation, and emergency rescue (6%). Out of pocket expenditure is typically financed by household revenues (71%) (see Figure 4).

Note that 86% of rural population and 82% of urban population are not covered under any scheme of health expenditure support. Due to high out of pocket healthcare expenditure, about 7% population is pushed below the poverty threshold every year.
Out of the total number of persons covered under health insurance in India, three-fourths are covered under government sponsored health schemes and the balance one-fourth are covered by private insurers. With respect to the government sponsored health insurance, more claims have been made in comparison to the premiums collected, i.e., the returns to the government have been negative.
It is in this context that the newly proposed National Health Protection Mission will be implemented. First, the scheme seeks to provide coverage for hospitalisation at the secondary and tertiary levels of healthcare. The High Level Expert Group set up by the Planning Commission (2011) recommended that the focus of healthcare provision in the country should be towards providing primary health care. It observed that focus on prevention and early management of health problems can reduce the need for complicated specialist care provided at the tertiary level. Note that depending on the level of care required, health institutions in India are broadly classified into three types: primary care (provided at primary health centres), secondary care (provided at district hospitals), and tertiary care institutions (provided at specialised hospitals like AIIMS).
Second, the focus of the Mission seems to be on hospitalisation (including pre and post hospitalisation charges). However, most of the out of the pocket expenditure made by consumers is actually on buying medicines (52%) as seen in Figure 3. Further, these purchases are mostly made for patients who do not need hospitalisation.