
Applications for the LAMP Fellowship 2025-26 will open soon. Sign up here to be notified when the dates are announced.
The central government has enforced a nation-wide lockdown between March 25 and May 3 as part of its measures to contain the spread of COVID-19. During the lockdown, several restrictions have been placed on the movement of individuals and economic activities have come to a halt barring the activities related to essential goods and services. The restrictions are being relaxed in less affected areas in a limited manner since April 20. In this blog, we look at how the lockdown has impacted the demand and supply of electricity and what possible repercussions its prolonged effect may have on the power sector.
Power supply saw a decrease of 25% during the lockdown (year-on-year)
As electricity cannot be stored in large amount, the power generation and supply for a given day are planned based on the forecast for demand. The months of January and February in 2020 had seen an increase of 3% and 7% in power supply, respectively as compared to 2019 (year-on-year). In comparison, the power supply saw a decrease of 3% between March 1 and March 24. During the lockdown between March 24 and April 19, the total power supply saw a decrease of about 25% (year-on-year).
Figure 1: % change in power supply position between March 1 and April 19 (Y-o-Y from 2019 to 2020)

Sources: Daily Reports; POSOCO; PRS.
If we look at the consumption pattern by consumer category, in 2018-19, 41% of total electricity consumption was for industrial purposes, followed by 25% for domestic and 18% for agricultural purposes. As the lockdown has severely reduced the industrial and commercial activities in the country, these segments would have seen a considerable decline in demand for electricity. However, note that the domestic demand may have seen an uptick as people are staying indoors.
Figure 2: Power consumption by consumer segment in 2018-19
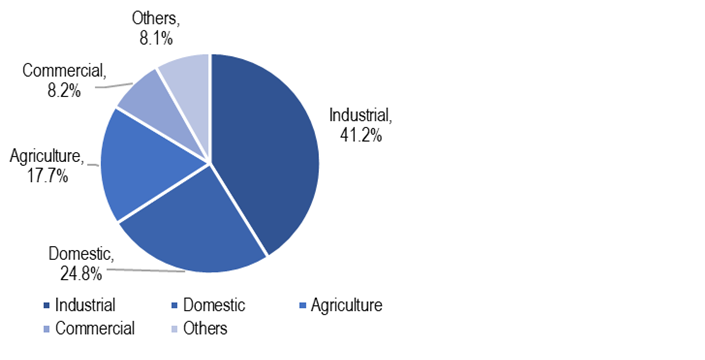
Sources: Central Electricity Authority; PRS.
Electricity demand may continue to be subdued over the next few months. At this point, it is unclear that when lockdown restrictions are eased, how soon will economic activities return to pre COVID-19 levels. India’s growth projections also highlight a slowdown in the economy in 2020 which will further impact the demand for electricity. On April 16, the International Monetary Fund has slashed its projection for India’s GDP growth in 2020 from 5.8% to 1.9%.
A nominal increase in energy and peak deficit levels
As power sector related operations have been classified as essential services, the plant operations and availability of fuel (primarily coal) have not been significantly constrained. This can be observed with the energy deficit and peak deficit levels during the lockdown period which have remained at a nominal level. Energy deficit indicates the shortfall in energy supply against the demand during the day. The average energy deficit between March 25 and April 19 has been 0.42% while the corresponding figure was 0.33% between March 1 and March 24. Similarly, the average peak deficit between March 25 and April 19 has been 0.56% as compared to 0.41% between March 1 and March 24. Peak deficit indicates the shortfall in supply against demand during highest consumption period in a day.
Figure 3: Energy deficit and peak deficit between March 1, 2020 and April 19, 2020 (in %)

Sources: Daily Reports; POSOCO; PRS.
Coal stock with power plants increases
Coal is the primary source of power generation in the country (~71% in March 2020). During the lockdown period, the coal stock with coal power plants has seen an increase. As of April 19, total coal-stock with the power plants in the country (in days) has risen to 29 days as compared to 24 days on March 24. This indicates that the supply of coal has not been constrained during the lockdown, at least to the extent of meeting the requirements of power plants.
Energy mix changes during the lockdown, power generation from coal impacted
During the lockdown, power generation has been adjusted to compensate for reduced consumption, Most of this reduction in consumption has been adjusted by reduced coal power generation. As can be seen in Table 1, coal power generation reduced from an average of 2,511 MU between March 1 and March 24 to 1,873 MU between March 25 and April 19 (about 25%). As a result, the contribution of coal in total power generation reduced from an average of 72.5% to 65.6% between these two periods.
Table 1: Energy Mix during March 1-April 19, 2020

Sources: Daily Reports; POSOCO; PRS.
This shift may be happening due to various reasons including: (i) renewable energy sources (solar, wind, and small hydro) have MUST RUN status, i.e., the power generated by them has to be given the highest priority by distribution companies, and (ii) running cost of renewable power plants is lower as compared to thermal power plants.
This suggests that if growth in electricity demand were to remain weak, the adverse impact on the coal power plants could be more as compared to other power generation sources. This will also translate into weak demand for coal in the country as almost 87% of the domestic coal production is used by the power sector. Note that the plant load factor (PLF) of the thermal power plants has seen a considerable decline over the years, decreasing from 77.5% in 2009-10 to 56.4% in 2019-20. Low PLF implies that coal plants have been lying idle. Coal power plants require significant fixed costs, and they incur such costs even when the plant is lying idle. The declining capacity utilisation augmented by a weaker demand will undermine the financial viability of these plants further.
Figure 4: Power generation from coal between March 1, 2020 and April 19, 2020 (in MU)
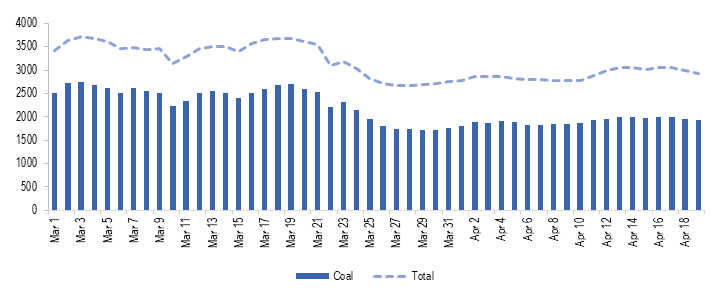
Sources: Daily Reports; POSOCO; PRS.
Finances of the power sector to be severely impacted
Power distribution companies (discoms) buy power from generation companies and supply it to consumers. In India, most of the discoms are state-owned utilities. One of the key concerns in the Indian power sector has been the poor financial health of its discoms. The discoms have had high levels of debt and have been running losses. The debt problem was partly addressed under the UDAY scheme as state governments took over 75% of the debt of state-run discoms (around 2.1 lakh crore in two years 2015-16 and 2016-17). However, discoms have continued to register losses owing to underpricing of electricity tariff for some consumer segments, and other forms of technical and commercial losses. Outstanding dues of discoms towards power generation companies have also been increasing, indicating financial stress in some discoms. At the end of February 2020, the total outstanding dues of discoms to generation companies stood at Rs 92,602 crore.
Due to the lockdown and its further impact in the near term, the financial situation of discoms is likely to be aggravated. This will also impact other entities in the value chain including generation companies and their fuel suppliers. This may lead to reduced availability of working capital for these entities and an increase in the risk of NPAs in the sector. Note that, as of February 2020, the power sector has the largest share in the deployment of domestic bank credit among industries (Rs 5.4 lakh crore, 19.3% of total).
Following are some of the factors which have impacted the financial situation during the lockdown:
Reduced cross-subsidy: In most states, the electricity tariff for domestic and agriculture consumers is lower than the actual cost of supply. Along with the subsidy by the state governments, this gap in revenue is partly compensated by charging industrial and commercial consumers at a higher rate. Hence, industrial and commercial segments cross-subsidise the power consumption by domestic and agricultural consumers.
The lockdown has led to a halt on commercial and industrial activities while people are staying indoors. This has led to a situation where the demand from the consumer segments who cross-subsidise has decreased while the demand from consumer segments who are cross-subsidised has increased. Due to this, the gap between revenue realised by discoms and cost of supply will widen, leading to further losses for discoms. States may choose to bridge this gap by providing a higher subsidy.
Moratorium to consumers: To mitigate the financial hardship of citizens due to COVID-19, some states such as Rajasthan, Uttar Pradesh, and Goa, among others, have provided consumers with a moratorium for payment of electricity bills. At the same time, the discoms are required to continue supplying electricity. This will mean that the return for the supply made in March and April will be delayed, leading to lesser cash in hand for discoms.
Some state governments such as Bihar also announced a reduction in tariff for domestic and agricultural consumers. Although, the reduction in tariff will be compensated to discoms by government subsidy.
Constraints with government finances: The revenue collection of states has been severely impacted as economic activities have come to a halt. Further, the state governments are directing their resources for funding relief measures such as food distribution, direct cash transfers, and healthcare. This may adversely affect or delay the subsidy transfer to discoms.
The UDAY scheme also requires states to progressively fund greater share in losses of discoms from their budgetary resources (10% in 2018-19, 25% in 2019-20, and 50% in 2020-21). As losses of discoms may widen due to the above-mentioned factors, the state government’s financial burden is likely to increase.
Capacity addition may be adversely impacted
As per the National Electricity Plan, India’s total capacity addition target is around 176 GW for 2017-2022. This comprises of 118 GW from renewable sources, 6.8 GW from hydro sources, and 6.4 GW from coal (apart from 47.8 GW of coal-based power projects already in various stages of production as of January 2018).
India has set a goal of installing 175 GW of Renewable Power Capacity by 2022 as part of its climate change commitments (86 GW has been installed as of January 2020). In January 2020, the Parliamentary Standing Committee on Energy observed that India could only install 82% and 55% of its annual renewable energy capacity addition targets in 2017-18 and 2018-19. As of January 2020, 67% of the target has been achieved for 2019-20.
Due to the impact of COVID-19, the capacity addition targets for various sources is likely to be adversely impacted in the short run as:
construction activities were stopped during the lockdown and will take some time to return to normal,
disruption in the global supply chain may lead to difficulties with the availability of key components leading to delay in execution of projects, for instance, for solar power plants, solar PV modules are mainly imported from China, and
reduced revenue for companies due to weak demand will leave companies with less capacity left for capital expenditure.
Key reforms likely to be delayed
Following are some of the important reforms anticipated in 2020-21 which may get delayed due to the developing situation:
The real-time market for electricity: The real-time market for electricity was to be operationalised from April 1, 2020. However, the lockdown has led to delay in completion of testing and trial runs. The revised date for implementation is now June 1, 2020.
UDAY 2.0/ADITYA: A new scheme for the financial turnaround of discoms was likely to come this year. The scheme would have provided for the installation of smart meters and incentives for rationalisation of the tariff, among other things. It remains to be seen what this scheme would be like since the situation with government finances is also going to worsen due to anticipated economic slowdown.
Auction of coal blocks for commercial mining: The Coal Ministry has been considering auction of coal mines for commercial mining this year. 100% FDI has been allowed in the coal mining activity for commercial sale of coal to attract foreign players. However, the global economic slowdown may mean that the auctions may not generate enough interest from foreign as well as domestic players.
For a detailed analysis of the Indian Power Sector, please see here. For details on the number of daily COVID-19 cases in the country and across states, please see here. For details on the major COVID-19 related notifications released by the centre and the states, please see here.
The National Medical Commission (NMC) Bill, 2017 was introduced in Lok Sabha in December, 2017. It was examined by the Standing Committee on Health, which submitted its report during Budget Session 2018. The Bill seeks to regulate medical education and practice in India. In this post, we analyse the Bill in its current form.
How is medical education and practice regulated currently?
The Medical Council of India (MCI) is responsible for regulating medical education and practice. Over the years, there have been several issues with the functioning of the MCI with respect to its regulatory role, composition, allegations of corruption, and lack of accountability. For example, MCI is an elected body where its members are elected by medical practitioners themselves, i.e. the regulator is elected by the regulated. In light of such issues, experts recommended nomination based constitution of the MCI instead of election, and separating the regulation of medical education and medical practice. They suggested that legislative changes should be brought in to overhaul the functioning of the MCI.
To meet this objective, the Bill repeals the Indian Medical Council Act, 1956 and dissolves the current Medical Council of India (MCI) which regulates medical education and practice.
Who will be a part of the NMC?
The NMC will consist of 25 members, of which at least 17 (68%) will be medical practitioners. The Standing Committee has noted that the current MCI is non-diverse and consists mostly of doctors who look out for their own self-interest over larger public interest. In order to reduce the monopoly of doctors, it recommended that the MCI should include diverse stakeholders such as public health experts, social scientists, and health economists. In other countries, such as the United Kingdom, the General Medical Council (GMC) responsible for regulating medical education and practice consists of 12 medical practitioners and 12 lay members (such as community health members, and administrators from the local government).
How will the issues of medical misconduct be addressed?
The State Medical Council will receive complaints relating to professional or ethical misconduct against a registered doctor. If the doctor is aggrieved by the decision of the State Medical Council, he may appeal to the Ethics and Medical Registration Board, and further before the NMC. Appeals against the decision of the NMC will lie before the central government. It is unclear why the central government is an appellate authority with regard to such matters.
It may be argued that disputes related to ethics and misconduct in medical practice may require judicial expertise. For example, in the UK, the GMC receives complaints with regard to ethical misconduct and is required to do an initial documentary investigation. It then forwards the complaint to a Tribunal, which is a judicial body independent of the GMC. The adjudication and final disciplinary action is decided by the Tribunal.
What will the NMC’s role be in fee regulation of private medical colleges?
In India, the Supreme Court has held that private providers of education have to operate as charitable and not for profit institutions. Despite this, many private education institutions continue to charge exorbitant fees which makes medical education unaffordable and inaccessible to meritorious students. Currently, for private unaided medical colleges, the fee structure is decided by a committee set up by state governments under the chairmanship of a retired High Court judge. The Bill allows the NMC to frame guidelines for determination of fees for up to 40% of seats in private medical colleges and deemed universities. The question is whether the NMC as a regulator should regulate fees charged by private medical colleges.
A NITI Aayog Committee (2016) was of the opinion that a fee cap would discourage the entry of private colleges, therefore, limiting the expansion of medical education. It also observed that it is difficult to enforce such a fee cap and could lead medical colleges to continue charging high fees under other pretexts.
Note that the Parliamentary Standing Committee (2018) which examined the Bill has recommended continuing the current system of fee structures being decided by the Committee under the chairmanship of a retired High Court judge. However, for those private medical colleges and deemed universities, unregulated under the existing mechanism, fee must be regulated for at least 50% of the seats. The Union Cabinet has approved an Amendment to increase the regulation of fees to 50% of seats.
How will doctors become eligible to practice?
The Bill introduces a National Licentiate Examination for students graduating from medical institutions in order to obtain a licence to practice as a medical professional.
However, the NMC may permit a medical practitioner to perform surgery or practice medicine without qualifying the National Licentiate Examination, in such circumstances and for such period as may be specified by regulations. The Ministry of Health and Family Welfare has clarified that this exemption is not meant to allow doctors failing the National Licentiate Examination to practice but is intended to allow medical professionals like nurse practitioners and dentists to practice. It is unclear from the Bill that the term ‘medical practitioner’ includes medical professionals (like nurses) other than MBBS doctors.
Further, the Bill does not specify the validity period of this licence to practice. In other countries such as the United Kingdom and Australia, a licence to practice needs to be periodically renewed. For example, in the UK the licence has to be renewed every five years, and in Australia it has to renewed annually.
What are the issues around the bridge course for AYUSH practitioners to prescribe modern medicine?
The debate around AYUSH practitioners prescribing modern medicine
There is a provision in the Bill which states that there may be a bridge course which AYUSH practitioners (practicing Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homoeopathy) can undertake in order to prescribe certain kinds of modern medicine. There are differing views on whether AYUSH practitioners should prescribe modern medicines.
Over the years, various committees have recommended a functional integration among various systems of medicine i.e. Ayurveda, modern medicine, and others. On the other hand, experts state that the bridge course may promote the positioning of AYUSH practitioners as stand-ins for allopathic doctors owing to the shortage of doctors across the country. This in turn may affect the development of AYUSH systems of medicine as independent systems of medicine.
Moreover, AYUSH doctors do not have to go through any licentiate examination to be registered by the NMC, unlike the other doctors. Recently, the Union Cabinet has approved an Amendment to remove the provision of the bridge course.
Status of other kinds of medical personnel
As of January 2018, the doctor to population ratio in India was 1:1655 compared to the World Health Organisation standard of 1:1000. The Ministry of Health and Family Welfare stated that the introduction of the bridge course for AYUSH practitioners under the Bill will help fill in the gaps of availability of medical professionals.
If the purpose of the bridge course is to address shortage of medical professionals, it is unclear why the option to take the bridge course does not apply to other cadres of allopathic medical professionals such as nurses, and dentists. There are other countries where medical professionals other than doctors are allowed to prescribe allopathic medicine. For example, Nurse Practitioners in the USA provide a full range of primary, acute, and specialty health care services, including ordering and performing diagnostic tests, and prescribing medications. For this purpose, Nurse Practitioners must complete a master’s or doctoral degree program, advanced clinical training, and obtain a national certification.