
The National Medical Commission Bill, 2017 was introduced in Lok Sabha recently and is listed for consideration and passage today.[1] The Bill seeks to regulate medical education and practice in India. To meet this objective, the Bill repeals the Indian Medical Council Act, 1956 and dissolves the current Medical Council of India (MCI). The MCI was established under the 1956 Act, to establish uniform standards of higher education qualifications in medicine and regulating its practice.[2]
A Committee was set up in 2016, under the NITI Aayog with Dr. Arvind Panagariya as its chair, to review the 1956 Act and recommend changes to improve medical education and the quality of doctors in India.[3] The Committee proposed that the Act be replaced by a new law, and also proposed a draft Bill in August 2016.
This post looks at the key provisions of the National Medical Commission Bill, 2017 introduced in Lok Sabha recently, and some issues which have been raised over the years regarding the regulation of medical education and practice in the country.
What are the key issues regarding the regulation of medical education and practice?
Several experts have examined the functioning of the MCI and suggested a different structure and governance system for its regulatory powers.3,[4] Some of the issues raised by them include:
Separation of regulatory powers
Over the years, the MCI has been criticised for its slow and unwieldy functioning owing to the concentration and centralisation of all regulatory functions in one single body. This is because the Council regulates medical education as well as medical practice. In this context, there have been recommendations that all professional councils like the MCI, should be divested of their academic functions, which should be subsumed under an apex body for higher education to be called the National Commission for Higher Education and Research.[5] This way there would be a separation between the regulation of medical education from regulation of medical practice.
An Expert Committee led by Prof. Ranjit Roy Chaudhury (2015), recommended structurally reconfiguring the MCI’s functions and suggested the formation of a National Medical Commission through a new Act.3 Here, the National Medical Commission would be an umbrella body for supervision of medical education and oversight of medial practice. It will have four segregated verticals under it to look at: (i) under-graduate medical education, (ii) post-graduate medical education, (iii) accreditation of medical institutions, and (iv) the registration of doctors. The 2017 Bill also creates four separate autonomous bodies for similar functions.
Composition of MCI
With most members of the MCI being elected, the NITI Aayog Committee (2016) noted the conflict of interest where the regulated elect the regulators, preventing the entry of skilled professionals for the job. The Committee recommended that a framework must be set up under which regulators are appointed through an independent selection process instead.
Fee Regulation
The NITI Aayog Committee (2016) recommended that a medical regulatory authority, such as the MCI, should not engage in fee regulation of private colleges. Such regulation of fee by regulatory authorities may encourage an underground economy for medical education seats with capitation fees (any payment in excess of the regular fee), in regulated private colleges. Further, the Committee stated that having a fee cap may discourage the entry of private colleges limiting the expansion of medical education in the country.
Professional conduct
The Standing Committee on Health (2016) observed that the present focus of the MCI is only on licensing of medical colleges.4 There is no emphasis given to the enforcement of medical ethics in education and on instances of corruption noted within the MCI. In light of this, the Committee recommended that the areas of medical education and medical practice should be separated in terms of enforcement of the appropriate ethics for each of these stages.
What does the National Medical Commission, 2017 Bill seek do to?
The 2017 Bill sets up the National Medical Commission (NMC) as an umbrella regulatory body with certain other bodies under it. The NMC will subsume the MCI and will regulate the medical education and practice in India. Under the Bill, states will establish their respective State Medical Councils within three years. These Councils will have a role similar to the NMC, at the state level.
Functions of the NMC include: (i) laying down policies for regulating medical institutions and medical professionals, (ii) assessing the requirements of human resources and infrastructure in healthcare, (iii) ensuring compliance by the State Medical Councils with the regulations made under the Bill, and (iv) framing guidelines for determination of fee for up to 40% of the seats in the private medical institutions and deemed universities which are governed by the Bill.
Who will be a part of the NMC?
The NMC will consist of 25 members, appointed by the central government. It will include representatives from Indian Council of Medical Research, and Directorate General of Health Services. A search committee will recommend names to the central government for the post of Chairperson, and the part-time members. These posts will have a maximum term of four years, and will not be eligible for extension or reappointment.
What are the regulatory bodies being set up under the NMC?
The Bill sets up four autonomous boards under the supervision of the NMC, as recommended by various experts. Each autonomous board will consist of a President and two members, appointed by the central government (on the recommendation of the search committee). These bodies are:
What does the Bill say regarding the conduct of medical entrance examinations?
There will be a uniform National Eligibility-cum-Entrance Test (NEET) for admission to under-graduate medical education in all medical institutions governed by the Bill. The NMC will specify the manner of conducting common counselling for admission in all such medical institutions.
Further, there will be a National Licentiate Examination for the students graduating from medical institutions to obtain the license for practice. This Examination will also serve as the basis for admission into post-graduate courses at medical institutions.
————————————————————–
[1] The National Medical Commission Bill, 2017, http://www.prsindia.org/uploads/media/medical%20commission/National%20Medical%20Commission%20Bill,%202017.pdf.
[2] Indian Medical Council Act, 1933.
[3] A Preliminary Report of the Committee on the Reform of the Indian Medical Council Act, 1956, NITI Aayog, August 7, 2016, http://niti.gov.in/writereaddata/files/document_publication/MCI%20Report%20.pdf.
[4] “Report no. 92: Functioning of the Medical Council of India”, Standing Committee on Health and Family Welfare, March 8, 2016, http://164.100.47.5/newcommittee/reports/EnglishCommittees/Committee%20on%20Health%20and%20Family%20Welfare/92.pdf
[5] “Report of the Committee to Advise on Renovation and Rejuvenation of Higher Education”, Ministry of Human Resource Development, 2009, http://mhrd.gov.in/sites/upload_files/mhrd/files/document-reports/YPC-Report.pdf.
As of May 11, 2020, there are 67,152 confirmed cases of COVID-19 in India. Since May 4, 24,619 new cases have been registered. Out of the confirmed cases so far, 20,917 patients have been cured/discharged and 2,206 have died. As the spread of COVID-19 has increased across the country, the central government has continued to announce several policy decisions to contain the spread, and support citizens and businesses who are being affected by the pandemic. In this blog post, we summarise some of the key measures taken by the central government in this regard between May 4 and May 11, 2020.
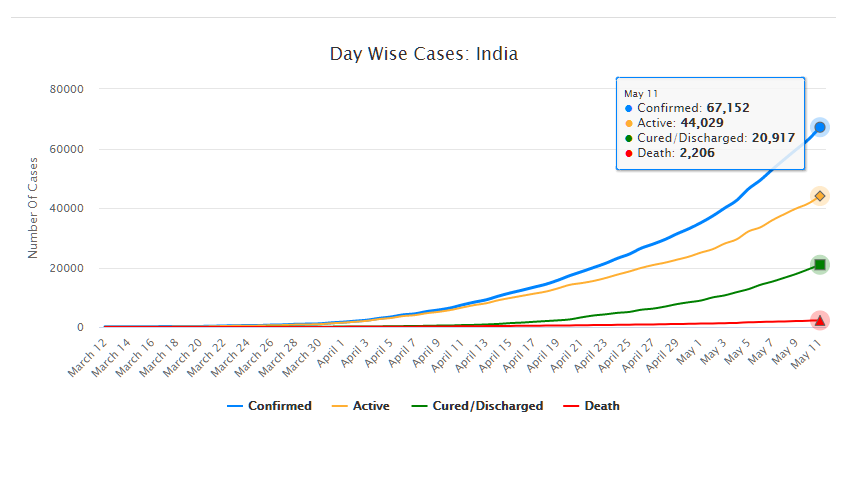
Source: Ministry of Health and Family Welfare; PRS.
Industry
Relaxation of labour laws in some states
The Gujarat, Himachal Pradesh, Rajasthan, Haryana, and Uttarakhand governments have passed notifications to increase maximum weekly work hours from 48 hours to 72 hours and daily work hours from 9 hours to 12 hours for certain factories. This was done to combat the shortage of labour caused by the lockdown. Further, some state governments stated that longer shifts would ensure a fewer number of workers in factories so as to allow for social distancing.
Madhya Pradesh has promulgated the Madhya Pradesh Labour Laws (Amendment) Ordinance, 2020. The Ordinance exempts establishments with less than 100 workers from adhering to the Madhya Pradesh Industrial Employment (Standing Orders) Act, 1961, which regulates the conditions of employment of workers. Further, it allows the state government to exempt any establishment or class of establishments from the Madhya Pradesh Shram Kalyan Nidhi Adhiniyam, 1982, which provides for the constitution of a welfare fund for labour.
The Uttar Pradesh government has published a draft Ordinance which exempts all factories and establishments engaged in manufacturing processes from all labour laws for a period of three years. Certain conditions will continue to apply with regard to payment of wages, safety, compensation and work hours, amongst others. However, labour laws providing for social security, industrial dispute resolution, trade unions, strikes, amongst others, will not apply under the Ordinance.
Financial aid
Central government signs an agreement with Asian Infrastructure Investment Bank for COVID-19 support
The central government and Asian Infrastructure Investment Bank (AIIB) signed a 500 million dollar agreement for the COVID-19 Emergency Response and Health Systems Preparedness Project. The project aims to help India respond to the COVID-19 pandemic and strengthen India’s public health system to manage future disease outbreaks. The project is being financed by the World Bank and AIIB in the amount of 1.5 billion dollars, of which one billion dollars is being provided by World Bank and 500 million dollars is being provided by AIIB. This financial support will be available to all states and union territories and will be used to address the needs of at-risk populations, medical personnel, and creating medical and testing facilities, amongst others. The project will be implemented by the National Health Mission, the National Center for Disease Control, and the Indian Council of Medical Research, under the Ministry of Health and Family Welfare.
Travel
Restarting of passenger travel by railways
Indian Railways plans to restart passenger trains from May 12 onwards. It will begin with 15 pairs of trains which will run from New Delhi station connecting Dibrugarh, Agartala, Howrah, Patna, Bilaspur, Ranchi, Bhubaneswar, Secunderabad, Bengaluru, Chennai, Thiruvananthapuram, Madgaon, Mumbai Central, Ahmedabad and Jammu Tawi. Booking for reservation in these trains will start at 4 pm on May 11. Thereafter, Indian Railways plans to start more services on new routes.
Return of Indians stranded abroad
The central government will facilitate the return of Indian nationals stranded abroad in a phased manner beginning on May 7. The travel will be arranged by aircraft and naval ships. The stranded Indians utilising the service will be required to pay for it. Medical screening of the passengers will be done before the flight. On reaching India, passengers will be required to download the Aarogya Setu app. Further, they will be quarantined by the concerned state government in either a hospital or a quarantine institution for 14 days on a payment basis. After quarantine, passengers will be tested for COVID-19 and further action will be taken based on the results.
For more information on the spread of COVID-19 and the central and state government response to the pandemic, please see here.